Writing this article has been surprisingly challenging. I have read every study I could get my hands on trying to find the direct action for the thyroid-melasma connection. In the beginning, I was confident I was making headway in my research. Day after frustrating day later I had to admit I simply could not find a link. The door to my investigation was finally slammed shut as there was no verifiable connection. I felt disheartened. I really thought I was working on something that could help melasma sufferers. I know I should be objective and not try to force conclusions from other people’s research, but I thought I was onto something. I still do, if I’m being honest. My gut tells me there is more to this story than meets the eye, and future research might reveal a direct connection.
While we know there is some interaction between the thyroid and melasma, there are too many conflicting studies to establish a causal link. Some studies show relationships between melasma patients and thyroid disorders, particularly autoimmunity, yet they are unable to pinpoint the hormonal mechanism in the thyroid that causes changes in skin pigmentation.
While researching this article I learned that hypothyroidism is the most overdiagnosed condition in the entire medical field. Thyroxine, a thyroid medication, is the second-highest of all prescribed medications. Thyroxine is the main hormone secreted into the bloodstream by the thyroid and is derived from synthetic or animal sources. Too much thyroid hormone can slow thyroid function.
Clearly, something is missing in the treatment of this condition. Micronutrients play a significant role in how the body utilizes and converts hormones, despite receiving little attention in conventional medicine. Micronutrient deficiencies can lead to low-functioning processes in the body. Diet is the foundation of health, and we are now discovering how important gut and liver function is to overall well-being.
Listen to this podcast to learn more about The Over-Diagnosis Of Hypothyroidism with three Functional Medicine doctors.
The thyroid is a small gland shaped like a butterfly in the base of your neck. It produces hormones that affect health and all aspects of metabolism. Levels of thyroid hormones can change your skin's appearance and function. The skin has thyroid hormone receptors that regulate epidermal cells and influence homeostasis. This relationship is why I’m very interested in the possible connection between melasma and the thyroid.
I personally know several women with melasma who also have thyroid disorders. In addition to skin health, hair loss, and brittle nails are both associated with thyroid function. Alopecia, an autoimmune disorder that causes hair loss, may also have a relationship with the thyroid. Studies indicate a possible correlation though they are ultimately inconclusive.
Melasma is often associated with Grave’s disease and Hashimoto’s patients. There seems to be a lot of correlation between melasma and hyperthyroidism and hypothyroidism, yet there is no conclusive causal link between thyroid hormone and melanogenesis. In my opinion, more work needs to be done on this topic. I hope that science leads to a better understanding of the thyroid-melasma connection if it truly exists.
Hypothalamus-Pituitary-Thyroid Axis.
Many of the hormonal mechanisms described here were also mentioned in my Stress And Your Skin article because the HPA axis is very closely connected to thyroid function. This is called the HPT Axis (hypothalamus-pituitary-thyroid axis). I suggest reviewing the article to help unpack the more dense medical jargon below.
The hypothalamus makes a thyrotropin-releasing hormone (TRH), the same pathway that produces CRH. TRH then stimulates the pituitary gland to make a thyroid-stimulating hormone (TSH). TRH acts directly on the pigmentation of hair but has not been shown to act directly on skin pigmentation. There is some evidence that high levels of TSH can increase the levels of ACTH, the primary hormone that controls pigmentation in the skin. Too much ACTH can increase pigmentation in the skin and cause melasma. Both TSH and ACTH are derived from the same melanogenic pathway, also associated with melasma.
Knowing how the HPA axis plays a critical role in melasma, it seems that the HPT axis could possibly influence the HPA axis. This could be the connection between melasma and thyroid function and I’d love to see more research on this topic. For now, it is only my personal speculation.
Micronutrients.
There are several nutrients that play a role in thyroid function. Without these nutrients, the body will have a harder time producing thyroid hormones which need to be processed and converted into other hormones for the thyroid to be at its healthiest.
Iodine is needed for thyroid hormone production. The body doesn’t make iodine, so supplementation is important. Hypothyroidism is often associated with iodine deficiency.
Selenium is important for thyroid metabolism and regulation, a deficiency in selenium can cause a low-functioning thyroid.
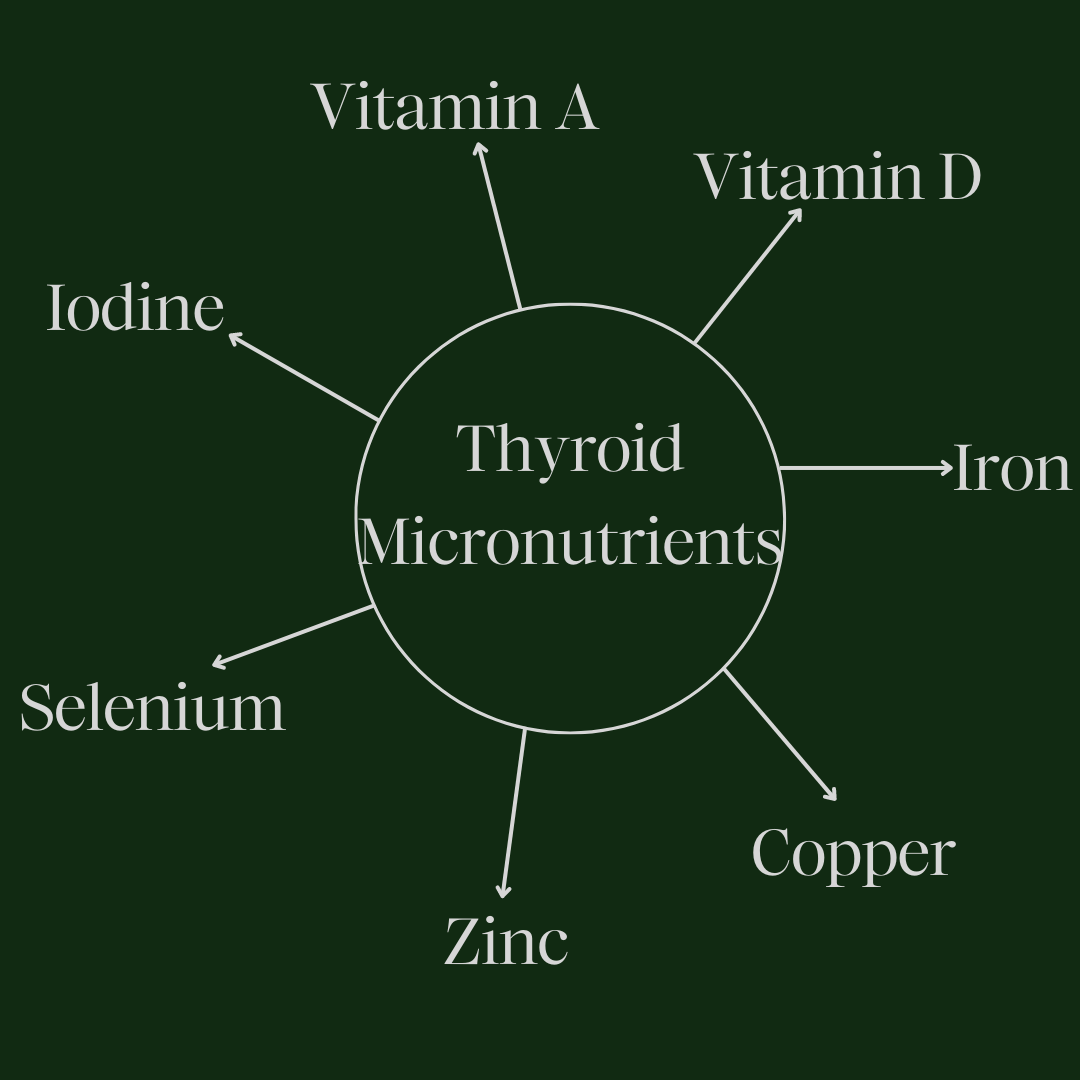
Zinc promotes TSH production, T4, and T3 and assists in T4 and T3 conversion.
Copper balances zinc and assists in T4 production and regulates absorption.
Iron converts T4 into its active form of thyroid hormone. Anemia can cause hypothyroidism, this is probably one of the most important minerals for thyroid function.
Another thing to note is that checking your ferritin levels is more important than checking your iron levels. Ferritin is a protein inside of your cells that stores iron. Think of it as your iron reserve, so measuring it gives you a better idea of where your iron levels are at. If ferritin is low then you need more ferritin, not iron. Understanding this is very important for resolving anemia properly.
Iron is another controversial topic in the melasma world. Some studies show a connection between iron deficiency and melasma while others disagree and claim no association. Still, iron overload promotes melanogenesis and can cause hyperpigmentation. Conversely, iron deficiency usually appears as pale skin and dark circles around the eyes.
Vitamin D helps regulate TSH levels.
Vitamin A regulates thyroid hormone metabolism and lowers TSH.
As you can see, many of these important micronutrients are essential for optimum thyroid function. A deficiency in one or more of those listed above can contribute to an underactive thyroid.
Thyroid-Gut Axis.
The thyroid-gut axis is tremendously important for thyroid optimization. A healthy gut is important for vitamin and mineral absorption. There is a clear link between micronutrient deficiency and thyroid dysfunction.
Hashimoto’s Disease is a form of thyroid autoimmunity that can result in an under-functioning thyroid. Leaky gut syndrome, simply a damaged intestinal barrier, is extremely common. This allows toxins to pass through the gut lining and stimulate the immune system, particularly the production of antibodies. Gut dysbiosis contributes to the development of Hashimoto’s, which is why these two imbalances often go hand in hand.
T4 and T3 have been shown to protect the gut’s mucosal lining from stress-induced ulcers. These hormones also protect the gut from accumulating too much inflammation. The microbiome assists in the conversion of T4 to active T3 and the gut also assists in thyroid hormone metabolism.
Stress can also affect thyroid hormone in the gut by suppressing active T3, rendering it inactive.
When gut dysbiosis occurs, harmful bacteria (pathogens) can colonize the gut. Not only does this feed systemic inflammation, but there is a direct correlation between thyroid cancer, nodules, and the gut microbiome. The gut microbiome keeps pathogens at bay and lowers inflammation—two vital factors for thyroid function & health.
Thyroid-Liver Connection.
Toxin buildup is the primary reason for thyroid autoimmunity. The thyroid-liver relationship is similar to the thyroid-gut relationship. The thyroid depends on the liver for complete homeostasis. In fact, several liver diseases have been directly linked to thyroid dysfunction. The liver converts 80% of T4 into T3. If hypothyroidism goes untreated the result can be fatty liver disease and hepatic fibrosis.
A small study has shown that 62% of Hashimoto’s patients had low glutathione levels.
Low levels of glutathione are associated with high levels of TPO antibodies and high TSH. Glutathione is an important antioxidant that helps keep free radicals at bay. Free radicals are dangerous as they play an important role in the development of thyroid antibodies. Liver support is vital for healthy thyroid function.
In Conclusion.
Supporting your gut and liver with micronutrients and supplementation is incredibly important for thyroid function. Though there is currently no proven connection between the thyroid and melasma, healing the thyroid is an important step in overall health and well-being. I can’t help but shake the feeling that science will one day find a more direct link between thyroid hormone and melasma specifically.
Resources:
https://www.frontiersin.org/articles/10.3389/fendo.2013.00104/full
https://www.journalijar.com/article/37320/thyroid-disorders-in-patients-with-melasma/
https://academic.oup.com/jcem/article-abstract/61/1/28/2674920?redirectedFrom=fulltext
https://www.ijced.org/journal-article-file/11138
https://www.sciencedirect.com/science/article/pii/S0022202X15345450
https://hero.epa.gov/hero/index.cfm/reference/details/reference_id/9304706
https://core.ac.uk/download/pdf/82222952.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6861141/
https://www.sciencedirect.com/science/article/pii/S1027811714000548
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166193/
https://pubmed.ncbi.nlm.nih.gov/23378454/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166193/
https://pubmed.ncbi.nlm.nih.gov/30584647/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7353203/
https://www.cell.com/trends/endocrinology-metabolism/fulltext/S1043-2760(19)30107-9
https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-022-02612-3


Leave a Reply