When it comes to chronic skin conditions, histamine is often overlooked. The melasma-histamine connection is not as common, but can still be a possibility and a contributing factor to melasma development and progression. In Defining Melasma I briefly mention how histamine can impact melasma, but let’s take a deeper look.
Melasma is a complex condition that varies from person to person, the way it should be treated will vary. These stubborn dark spots can appear anywhere on the body and can worsen with sun exposure. For a full explanation of what melasma is please see the Defining Melasma article. It's important to note that while histamine can be a primary cause of melasma development, it's often not the only thing contributing to the condition but many things simultaneously working against you.
Genetics could also be a factor in histamine-related melasma. However, with proper diet and supplementation, you can learn to manage it. Remember, having a genetic mutation doesn't mean you can't heal your melasma. It means you'll have to work harder to find the root cause. Be patient with yourself and the process!
Histamine.
Histamine is a chemical compound produced by the body that plays a vital role in several physiological processes. It is a biogenic amine that acts as a neurotransmitter and a local hormone. Histamine is synthesized by mast cells located throughout the body, especially in the skin, lungs, and GI tract. I mentioned this in The Gut & Skin article.
Histamine plays a critical role in the immune response system. When the body is exposed to an allergen or encounters tissue damage, histamine is released by immune cells, leading to a cascade of events that trigger the immune response. Histamine causes blood vessels to dilate and become more permeable, allowing immune cells to enter the affected tissue and fight off the infection or injury. Histamine also stimulates the production of pro-inflammatory cytokines.
Histamine plays a crucial role in the allergic response. When the body encounters an allergen, such as pollen or pet dander, immune cells release histamine as a response. The dilation of blood vessels leads to swelling and redness in the affected tissue. It also triggers the production of mucus, leading to symptoms such as sneezing and a runny nose. Additionally, histamine can stimulate nerve endings, leading to itching and other uncomfortable sensations.
Histamine also plays a significant role in the digestive system. It is released by cells in the stomach lining. It acts as a neurotransmitter to stimulate the production of stomach acid, which helps break down food and aids in digestion. However, excessive histamine in the stomach can lead to conditions such as peptic ulcers and acid reflux disease. In addition, to its role in the stomach, histamine is also involved in regulating gut function and immune responses in the intestines. Imbalances of histamine levels in the gut are linked to several digestive disorders, including inflammatory bowel disease and irritable bowel syndrome.
If you have read my previous article The Gut & Skin, you understand the significant role of the immune system and the gut in melasma. The melasma-histamine connection is critical in some cases.
Melasma-Histamine Connection.
Recent research has shown that histamine can play a role in the development of melasma. One study found that patients with melasma had more histamine in their skin than those without melasma. Additionally, the study found that histamine receptors were more abundant in the skin of patients with melasma.
Histamine can trigger melasma by stimulating the production of melanin in the skin. When histamine is released in response to an allergen or injury, it can cause the skin to become more sensitive to UV radiation. UV exposure also triggers the release of histamine from mast cells. When histamine binds to the H2 receptor, it activates the tyrosinase pathway and induces pigmentation.
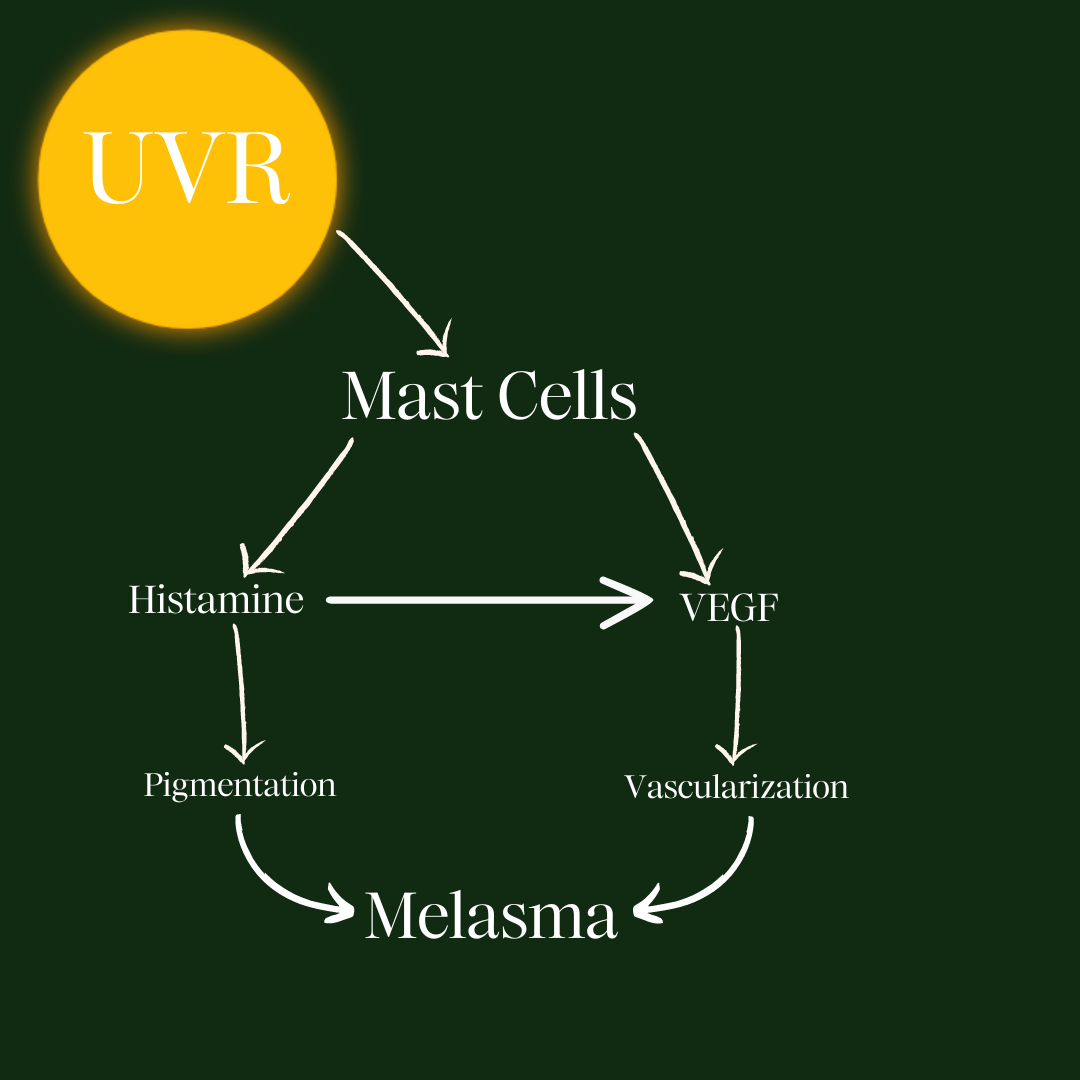
Melasma and histamine share an important characteristic, vascular endothelial growth factor (VEGF). VEGF is what stimulates the formation of new blood vessels. This process is called angiogenesis. VEGF is released from mast cells and causes hypervascularization. This explains why some people get visible tiny blood vessels in their pigmentation. In histamine, VEGF is involved in the allergic response. Histamine can stimulate the release of VEGF, leading to increased vascularity and swelling in the affected tissue. This can contribute to the symptoms such as itching, swelling, and redness.
On rare occasions, some have complained of itchy melasma, this could be an explanation for itchy pigmentation.
While the exact mechanisms of VEGF that contribute to the development of melasma and histamine are not fully understood, it is clear that VEGF plays a vital role in both conditions.
Histamine Intolerance.
Histamine intolerance is a condition where the body has difficulty breaking down and eliminating histamine, leading to a buildup of excess histamine. One possible genetic factor that may contribute to histamine intolerance is a mutation in the AOC1 gene, which codes for an enzyme called diamine oxidase (DAO). DAO is responsible for breaking down histamine in the body, and a mutation in the AOC1 gene can lead to reduced DAO activity and impaired histamine metabolism. This can result in a range of symptoms, including headaches, skin rash, itching, flushing, abdominal pain, and diarrhea, among others. While AOC1 gene mutations are not the only cause of histamine intolerance, identifying and addressing this genetic factor can be an important part of a comprehensive treatment plan for those with histamine intolerance.
The AOC1 gene could be one factor that gives melasma a genetic component, considering they are so closely related. However, I think it is possible to manage histamine and resolve melasma through several different avenues. The AOC1 gene is not the end for melasma sufferers. I firmly believe some genes can be turned off and on (epigenetics), making the condition express itself without symptoms.
Histamine intolerance can be complicated but, with the proper support, you can find relief.
Food And Histamine.
People with histamine intolerance often have reactions to certain high-histamine foods. Eliminating histamine foods until you find the root cause will help minimize aggravating your melasma. It won’t necessarily be a permanent lifestyle change. There are ways to manage the DAO gene once other mechanisms are repaired.
It's important to note that while some of these foods are high in histamine, not everyone who consumes them will experience symptoms. Histamine intolerance is a complex condition that can be influenced by a range of factors, including individual tolerance levels, gut health, and the presence of other dietary or lifestyle triggers. If you suspect you may be sensitive to histamine-rich foods, it's best to remove them from your diet until you can heal the root cause.
Conclusion.
The melasma-histamine connection is critical even if it isn’t a root cause for you it’s good to know what the possible connections there are. As that old saying goes, “Knowing is half the battle.”
I will be posting on IG and starting a public conversation about skin health. So keep your eyes peeled on my IG.



Leave a Reply